 How can a doctor look at you and tell you’re suffering from a chemical imbalance?
How can a doctor look at you and tell you’re suffering from a chemical imbalance?
(Spoiler alert!)
They can’t. And yet, the decision to alter the brain chemistry of 30 million Americans through the use of antidepressants is predicated on the belief that over the course of 20.8 minutes – the length of the average doctor visit – another human being can analyze the behavior of neurotransmitters in your brain just by looking at you.
Keep in mind that 42% of general practitioner appointments actually last less than 15 minutes. (Not that a 10-hour appointment would give your doctor enough time to develop x-ray vision and the capabilities of a functional magnetic resonance imaging brain scanner, but just sayin’.)
Wait a second
Why are we talking about general practitioners (i.e., your regular family doctor) if psychotropic drugs are involved? Oh, that’s right! Because 78% of patients who take antidepressants get their prescriptions from doctors who aren’t even psychiatrists!
Soooo, we have a few problems
And honestly, it’s hard to decide where to start. But let’s set aside that whole ‘doctors who weren’t trained to diagnose mental illness are diagnosing almost 80% of mental illnesses’ thing. And while we’re at it, go ahead and push pause on that pesky ‘how do you complete a thorough psychiatric assessment, issue a diagnosis and outline a comprehensive treatment plan in 20 minutes’ problem.
Instead, let’s get to the bottom of this chemical imbalance business. Because if you’re walking around and people can literally see everything your little chemicals are doing – well, then… that’s just awkward for everybody, isn’t it?
First off: Depression isn’t caused by a “chemical imbalance” (at least not one that’s understood yet)
 *Before we go any further, a quick disclaimer: The information presented in this post is in no way a dismissal of arguments claiming a biological basis for depression (I’m a huge believer in the role of genetics!) – rather, it is intended to support a more specific critique of the Serotonin Hypothesis and the use of pharmacological treatments to address depression based on the ill-defined and unsubstantiated theory of “chemical imbalance” .
*Before we go any further, a quick disclaimer: The information presented in this post is in no way a dismissal of arguments claiming a biological basis for depression (I’m a huge believer in the role of genetics!) – rather, it is intended to support a more specific critique of the Serotonin Hypothesis and the use of pharmacological treatments to address depression based on the ill-defined and unsubstantiated theory of “chemical imbalance” .
In 1965, a scientist by the name of Joseph Schildkraut hypothesized that depression was associated with low levels of norepinephrine – leading later researchers to theorize that serotonin was to blame. But here’s the catch: the theory never panned out. As Drs. Jeffrey R. Lacasse and Jonathan Leo explain,
Contemporary neuroscience research has failed to confirm any serotonergic lesion in any mental disorder, and has in fact provided significant counter-evidence to the explanation of a simple neurotransmitter deficiency.
As shocking as it sounds (given the pressure of antidepressant commercials conditioning us into the “chemical imbalance” mindset), the research has always been right in front of us: The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders – i.e., the manual doctors use to assess and diagnose mental disorders – does not list serotonin as the cause of any mental disorder. And, as Lacasse and Leo note: “The American Psychiatric Press Textbook of Clinical Psychiatry addresses serotonin deficiency as an unconfirmed hypothesis, stating, ‘Additional experience has not confirmed the monoamine depletion hypothesis’.”
Lacasse and Leo bring the point home:
While neuroscience is a rapidly advancing field, to propose that researchers can objectively identify a “chemical imbalance” at the molecular level is not compatible with the extant science. In fact, there is no scientifically established ideal “chemical balance” of serotonin, let alone an identifiable pathological imbalance.
(Emphasis added is my own.)
Wait – so how did this whole idea get so out of hand?!
Harvard Medical School lecturer and former New England Journal of Medicine editor-in-chief, Marcia Angell, offers a concise summary in her review of Robert Whitaker’s book, Anatomy of an Epidemic:
[T]hat theory had its genesis shortly after psychoactive drugs were introduced in the 1950s. The first was Thorazine (chlorpromazine), which was launched in 1954 as a “major tranquilizer” and quickly found widespread use in mental hospitals to calm psychotic patients, mainly those with schizophrenia. Thorazine was followed the next year by Miltown (meprobamate), sold as a “minor tranquilizer” to treat anxiety in outpatients. And in 1957, Marsilid (iproniazid) came on the market as a “psychic energizer” to treat depression.
In the space of three short years, then, drugs had become available to treat what at that time were regarded as the three major categories of mental illness—psychosis, anxiety, and depression—and the face of psychiatry was totally transformed. These drugs, however, had not initially been developed to treat mental illness. They had been derived from drugs meant to treat infections, and were found only serendipitously to alter the mental state.
(Emphasis added is my own.)
Angell goes on to note that fellow authors, Irving Kirsch (Associate Director of the Program of Placebo Studies at Harvard Medical School) and Daniel Carlat (Director of the Pew Prescription Project) – whose books are also reviewed in Angell’s essay – “[don’t] subscribe to the popular notion that mental illness is caused by a chemical imbalance in the brain” either:
When it was found that psychoactive drugs affect neurotransmitter levels in the brain, as evidenced mainly by the levels of their breakdown products in the spinal fluid, the theory arose that the cause of mental illness is an abnormality in the brain’s concentration of these chemicals that is specifically countered by the appropriate drug. For example, because Thorazine was found to lower dopamine levels in the brain, it was postulated that psychoses like schizophrenia are caused by too much dopamine. Or later, because certain antidepressants increase levels of the neurotransmitter serotonin in the brain, it was postulated that depression is caused by too little serotonin. […] Thus, instead of developing a drug to treat an abnormality, an abnormality was postulated to fit a drug.
That was a great leap in logic, as all three authors point out. It was entirely possible that drugs that affected neurotransmitter levels could relieve symptoms even if neurotransmitters had nothing to do with the illness in the first place (and even possible that they relieved symptoms through some other mode of action entirely). As Carlat puts it, “By this same logic one could argue that the cause of all pain conditions is a deficiency of opiates, since narcotic pain medications activate opiate receptors in the brain.” Or similarly, one could argue that fevers are caused by too little aspirin.
But the main problem with the theory is that after decades of trying to prove it, researchers have still come up empty-handed. All three authors document the failure of scientists to find good evidence in its favor.
(Emphasis added is my own.)
What it all means
Ok – so I know that was a TON of information, but the moral of the story is: depression and anxiety disorders are not caused by chemical imbalances – at least not ones that scientists understand. The second moral of the story is: even if they were, it’s literally impossible for anybody to just look at you and know that your problem is caused by anything having to do with brain chemistry. I mean, think about it: if you go to the doctor exhibiting signs of blood sugar problems, he/she doesn’t just write out a prescription for insulin and send you on your way! Physicians have absolutely no way of knowing what your blood sugar levels are – or if glucose is even the problem! – until they run some tests. So how on earth would they have any idea what’s going on with your brain chemistry when you walk into their office and tell them you’re sad? (And, for the record: there is no such thing as neuroimaging scans that can be used alone to diagnose mental illness.)
As Dr. Carlat notes,
We have no more than the most rudimentary understanding of the pathophysiology of mental illness and we have resorted to tenuous and ever-shifting theories of how our treatments work.
But the commercials say…
Now this is where stuff gets really interesting – and we’ll definitely talk more about this another day! – but for now I’ll leave you with a link to Lacasse & Leo’s article:
Serotonin and Depression: A Disconnect between the Advertisements and the Scientific Literature
Alright crew, that’s all for now!
But for anyone wanting to do a lil more investigating on their own – I can’t recommend Angell’s two essays (Part One, Part Two) and response letter enough! And if you haven’t already, check out this earlier Prayers and Apples post on Irving Kirsch. (You might also enjoy: Antidepressants Don’t Work For Most People, Doctors Agree, featuring Dr. Oz.)
Thanks so much for reading! If you enjoyed and/or learned something, I would really appreciate it if you’d consider sharing on Facebook, Twitter, etc. :) I think it’s really important that this information gets out there! To stay up to date on new posts, subscribe here! :)
Would love to hear your thoughts and questions!
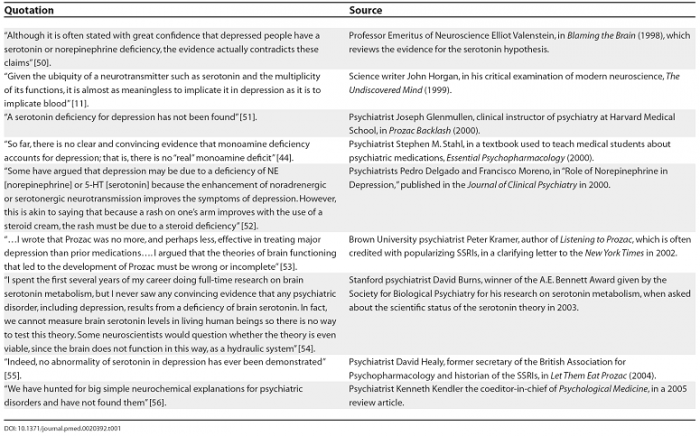
(And, in closing: here are a few great quotes organized by Lacasse and Leo!)
Resources
Angell, M. (2011 June 23). The Epidemic of Mental Illness: Why? The New York Review of Books. Retrieved: December 7, 2013.
Angell, M. (2011 July 14). The Illusions of Psychiatry. The New York Review of Books. Retrieved: December 7, 2013.
Coppen, A. (1967). The biochemistry of affective disorders. British Journal of Psychiatry, 113, pp. 1237-1264.
Lacasse, J.R. & Leo, J. (December 2005). Serotonin and Depression: A Disconnect between the Advertisements and the Scientific Literature. PLoS Medicine, 2 (12), p. e392.
Mark, T.L., Levit, K.R. & Buck, J.A. (September 2009). Data-points: psychotropic drug prescriptions by medical speciality. Pyschiatric Services, 60 (9), p. 1167.
Mojtabai, R. & Olfson, M. (2011). Proportion of Antidepressants Prescribed Without a Psychiatric Diagnosis Is Growing. Health Affairs, 30 (8), pp. 1434-1442.
National Center for Health Statistics. (2011). Antidepressant Use in Persons Aged 12 and Over: United States, 2005-2008. Centers for Disease Control and Prevention. Retrieved: December 8, 2013.
National Center for Health Statistics. (2010). National Ambulatory Medical Care Survey: 2010 Summary Tables. Centers for Disease Control and Prevention. Retrieved: December 8, 2013.
National Institute of Mental Health. (n.d.). Neuroimaging and Mental Illness: A Window Into the Brain. National Institutes of Health. Retrieved: December 8, 2013.
Oldham, J., Carlat, D., Friedman, R., Nirenberg, A. & Angell, M. (2011 July 14). The Illusions of Psychiatry: An Exchange. The New York Review of Books. Retrieved: December 7, 2013.
Schildkraut, J.J. (1965). The catecholamine hypothesis of affective disorders: A review of supporting evidence. The Journal of Neuropsychiatry and Clinical Neurosciences, 7, pp. 524-533.
Whitaker, R. (2010). Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America. New York: Crown.




GREAT article! ! even before I became a health conscious person, I knew prescribing these kinds of drugs based on a 15 minute conversation was wrong. I have great respect for doctors and even some for the pharmaceutical industry. But I do NOT like the ‘pusher’ mentality that has people blindly accepting the medical community’s push to get up on drugs to address symptoms instead of taking more time to find causes of illnesses. And, we should he our own health advocates and INSIST on more relevant answers. I get that from a commercial aspect, this method works great for the medical community, but what happened to the hypocratic oath? Many doctors have fallen for the ‘oakie doke’ and have either convinced themselves that this is ok, or they just don’t care….sad.
(Thanks so much! I always get nervous publishing these articles because, like you, I also have great respect for the medical community – so I never want my arguments to be miscontrued!) But this particular issue deserves a lot more transparency. And, like you said: patients need to start INSISTING on more relevant answers! Thanks so much for reading! :)
Wow hard to swallow that an entire educated nation has been so duped. You need to get this dialogue out – we certainly are rapidly becoming a nation on ” drugs”. Thanks for the excellent research!!
Glad you enjoyed! :) It’s definitely a touchy subject – as a lot of times people think you’re attacking the disorder itself (i.e., “People don’t need to take antidepressants because there’s nothing wrong with them!”) and that couldn’t be farther from the truth! My main motivation in promoting this type of info is weeding out treatment plans that don’t work, so that more attention can be focused on approaches that provide real, sustainable relief (without all the side-effects!). Thanks for taking the time to comment! :)
Another great article Jess, I always learn so much from you and have a giggle along the way ;) I had to re-post so I hope you dont mind. Take care and chat soon x
Are you kidding? A repost from you is like a blogging badge of honor ;) So glad to hear from you too – hope you’re doing well! :) xo