I know this isn’t exactly the sexiest comeback post, but I figured I owed you guys a more detailed explanation of why I’ve been too busy to blog! So, for better or worse, here’s Excuse Number One some of the research I’ve been working on:
Climate Change and the Risk of Heat-Related Deaths in Mood Disorder Patients Prescribed Antidepressants
1. Introduction
In 1997, two psychiatric patients died during a California heat wave. This fact alone is not that unusual. In a study conducted by the Centers for Disease Control and Prevention (1998), during 1979-1995, 6,615 deaths in the United States were attributed to excessive heat exposure. What makes the deaths of these two individuals especially significant is that the board-and-care facility where the patients were being treated was ordered to pay $1.2 million after their deaths for failing to disclose that heat intolerance was a potentially fatal side effect of their prescribed antipsychotic medication (Bark, 1998). My goal in introducing the following research is to prevent similar tragedies from occurring in the future.
General circulation models of climate change predict that heat waves will continue to become more frequent and intense (IPCC, 2007) – a pattern that poses a direct and urgent threat to individuals suffering from mental disorders. Evidence has shown that having a pre-existing psychiatric illness can more than triple the risk of death during a heat wave (Hansen, Bi, Nitschke, Ryan, Pisaniello & Tucker, 2008). While social factors unique to this population (i.e., lack of awareness, social isolation) can lead to heat-related morbidity and mortality (Berry, Bowen & Kjellstrom, 2010), I will instead focus on a contributory cause that offers the most potential for cost-effective intervention: psychiatric medication. More specifically, I will highlight the effect of extreme heat on mood disorder patients taking antidepressants. I will use establishment of this correlation, in light of urgent climate change predictions, to argue for immediate public policy adjustments within the medical field.
2. Antidepressants
Antidepressants are most commonly used in the treatment of unipolar and bipolar mood disorders. Butcher, Hooley & Mineka (2010) outline several categories of antidepressant medications:
Selective serotonin reuptake inhibitors (SSRIs)
- Most widely prescribed antidepressant
- Three medications from this category – flouxetine, sertaline and paroxetine (Prozac, Zoloft and Paxil) – were three of the eleven most prescribed drugs of any type in 2000 (Gitlin as cited in Butcher et al., 2010)
Tricyclics
- Drug treatment of choice prior to SSRIs, still widely prescribed
- Believed to be just as effective, if not more so, than SSRIs; however, tricyclics include more unpleasant side-effects (e.g, weight gain, dry mouth) and are highly toxic in large doses
Atypical drugs
- Examples include bupropion (Wellbutrin) and venlafaxine (Effexor)
- Gained popularity in the last decade
2.1 Heat and drug interaction
Body temperature is controlled by a complex regulatory system within the central nervous system that consists of various afferent and efferent pathways; the main neurotransmitters involved are serotonin and dopamine (Epstein, Albukrek, Kalmovitc, Moran & Shapiro, 1997). While serotonin neurotransmission mediates body temperature, a serotonin agonist decreases it (Wozniak, Aulakh, Hill & Murphy, 1988; Meltzer & Maes, 1995). The release of dopamine is also thought to regulate heat production and heat loss activities (Epstein et al., 1997). Importantly: these two neurotransmitters also play a crucial role in the pathology of mood disorders. Dopamine is involved with cognitive processing and pleasure; serotonin affects mood and behavior (Butcher et al., 2010).
 Recognizing the relationships between serotonin/dopamine and thermoregulation/thirst regulation and serotonin/dopamine and mood disorders, provides a general framework for understanding some of the ways in which antidepressant drugs (that manipulate serotonin/dopamine) could contribute to heat-related illness and/or death. Stollberger, Lutz & Finsterer (2009) offer a helpful overview:
Recognizing the relationships between serotonin/dopamine and thermoregulation/thirst regulation and serotonin/dopamine and mood disorders, provides a general framework for understanding some of the ways in which antidepressant drugs (that manipulate serotonin/dopamine) could contribute to heat-related illness and/or death. Stollberger, Lutz & Finsterer (2009) offer a helpful overview:
“Drugs interfere with thermoregulation at various levels. They affect the hypothalamic-set temperature, impede function of thermoreceptors, impair heat-production, impair the efficacy of the cholinergic system and thus sweat production, or may impede cutaneous vasodilatation” (p. 880).
While more studies are needed, it is believed that antidepressants may alter body temperature regulation via anti-dopaminergic action and impair sweating via anticholinergic action (Page, Hajat, Kovats & Howard, 2012). Kudoh, Takase & Takazawa (2003) note that antidepressants also have anticholinergic effects (which may affect sweat production/heat loss pathways). Postulations regarding interactions between heat and specific groups of antidepressant drugs are described below:
SSRIs
- SSRIs reduce serum sodium and, in turn, thirst (Stollberger et al., 2009); this could lead to accelerated dehydration during an extreme heat event.
Tricyclics
- The heat-intolerant effects of tricyclics may be due to their blocking effect on reuptake of norepinephrine and serotonin (Epstein et al., 1997).
Atypical drugs
- Fluoxetine (Prozac) may affect body temperature in two ways: enhanced heat production and inhibited heat loss. Fluoxetine inhibits the neural reuptake of serotonin. According to Epstein et al. (1997), since the release of serotonin in the anterior hypothalamus has been shown to stimulate cholinergic heat production pathways, inhibiting reuptake of serotonin will increase heat production. Also, since enhanced serotonin activity inhibits dopamineric heat loss pathways in the medial anterior hypothalamic preoptic area, the effect of fluoxetine on serotonin and dopamine levels might decrease heat loss (Epstein et al., 1997).
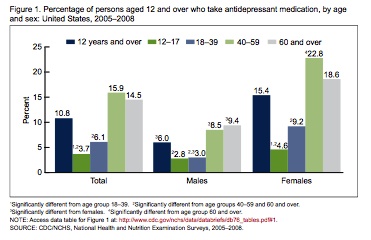
2.2 Usage and statistics
According to the National Center for Health Statistics, one in every ten Americans, aged 12 and over, now takes an antidepressant – an increase of almost 400% between 1988-1994 and 2005-2008 (Figure 1) (Pratt, Brody & Qiuping, 2011). More than 60% of Americans taking antidepressant medication have taken it for two years or longer, with 14% having taken the medication for ten years or more (Pratt et al., 2011).
3. Climate change
According to the UN Intergovernmental Panel on Climate Change (IPCC), warming of the climate is “unequivocal” (2007). This change will impact mood disorder patients prescribed antidepressants in two ways: through increases in global temperature and increased frequency of extreme heat events.
3.1 Temperature
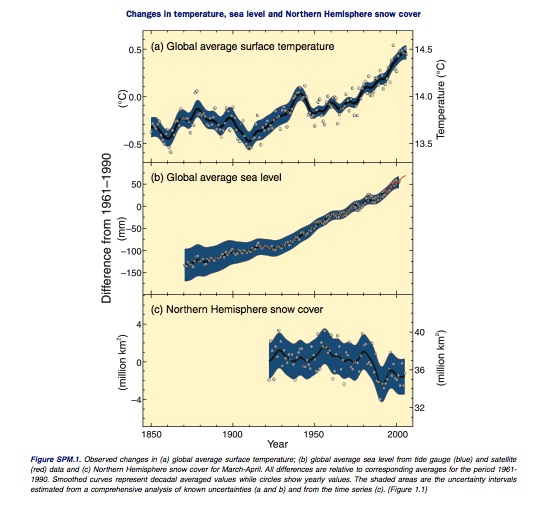
Studies show that not only have temperatures risen in the recent past, but they have done so at an alarming rate. According to the IPCC (2007), eleven of the twelve years spanning 1995-2006 rank among the twelve warmest years in the instrumental record of global surface temperature. Observations of these increases in global air and ocean temperatures, as well as widespread melting of snow/ice and rising global average sea level, are detailed in Figure 2.
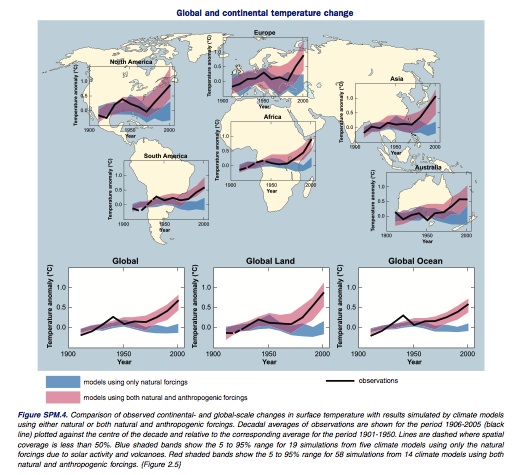
These observations aren’t limited to the recent past: average temperatures in the Northern Hemisphere during the second half of the 20th century are likely the highest temperatures in at least the past 1,300 years (IPCC, 2007). According to the IPCC (2007), this is very likely due to an increase in anthropogenic greenhouse gas (GHG) concentrations (Figure 3). Addressing future concerns, the IPCC (2007) notes that there is “high agreement and much evidence” that global GHG emissions will continue to grow over the next few decades – which would “very likely” result in changes during the 21st century that would be even larger than those observed during the 20th century.
More specifically: Climate model simulations project that for the first half of the 21st century, year-round temperatures in North America will warm approximately 1-3°C; annual warming, at high latitudes, is expected to increase more than 5°C by later in the century (Ruosteenoja, Carter, Jylha & Tuomenvirta, 2003 as cited in Luber & McGeehin, 2008).
3.2 Extreme heat events
Extreme heat events, or heat waves, are characterized by stagnant, warm air masses and consecutive nights with high minimum temperatures (Luber & McGeehin, 2008). In 2004, extreme heat events were responsible for more annual deaths than hurricanes, lightning, tornadoes, floods and earthquakes combined – making them the most prominent cause of weather-related human mortality in the U.S. (Luber & McGeehin, 2008). According to the IPCC (2007), North American cities that currently experience heat waves are expected to experience an increased number, intensity and duration of heat waves during the course of this century.
Ruosteenoja Carter et al. (2003 as cited in Luber & McGeehin, 2008) claim that the “significant upward trend” in the frequency of U.S. heat waves from 1949 to 1995 indicates an approximately 20% overall increase in the number of heat waves during that period. As Luber & McGeehin (2008) note, general circulation models project that during 2080-2099, Chicago will experience a 25% increase in heat waves and that during 2070-2099, the annual number of heat wave days in Los Angeles will increase from 12 to 44–95.
4. Studies
I have summarized several globally diverse studies that elucidate the role of antidepressants in the development of heat-related illness and/or death. While research in this field is limited, there is a growing interest in the relationship between climate change and psychiatric practices (Doherty & Clayton, 2011).
4.1 New York City, 1998
Bark (1998) compared deaths of patients in New York City psychiatric hospitals during heat waves from 1950 to 1984 with the overall New York City population and found that psychiatric patients had twice the risk of dying than the general public. (During this time, maximum temperatures ranged from 91 to 107°F). Bark (1998) also found that the risk for patients was highest in the 1970s, when higher dosages of antipsychotic medication were commonly used. Bark claims that his study shows that not only are psychiatric patients at increased risk during extreme heat events, but that such deaths are preventable.
4.2 Japan, 2003
Kudoh, Takase & Takazawa (2003) investigated temperature regulation during anesthesia and postoperative shivering in depression patients taking antidepressant drugs. Their results show that while intraoperative core hypothermia was decreased, patients taking antidepressants exhibited significantly more shivering. This suggests alterations in central thermoregulation attributable to antidepressant drug use (specifically: serotonergic receptor down-regulation) (Kudoh, et al., 2003).
4.3 France, 2009
During the 2003 French heat wave, 4,934 victims died of heat-related causes in twenty days (Stollberger et al., 2009). After hypothesizing that impaired thermoregulation and suppressed thirst were attributable to drug side effects (including those caused by antidepressants), Stollberger et al. (2009) concluded that insufficient water intake, impaired thermoregulation and resulting death may be directly linked to the use of certain drugs.
4.3.1 France, 2007
An earlier, smaller study of the same August 2003 heat wave produced similar results. Studying 56 patients admitted to a French emergency room with heat-related pathology, Martin-Latry, Goumy, Latry, Gabinski, Begaud, Faure & Verdoux (2007) found that nearly 40% of the patients used anxiety medication and nearly one-third took antidepressants. This led Martin-Latry et al. (2007) to conclude that antipsychotic drug use (including antidepressants) is an independent risk factor for hospitalization of heat-related pathologies during extreme heat events.
4.4 Britain, 2012
Analyzing a nationally representative primary care cohort study, Page, Hajat, Kovats, & Howard (2012) concluded that, “Prescribed psychotropic medication was found to modify the relationship between temperature and relative risk of death” (p. 487). Antipsychotic medications were associated with a 7% increase in relative risk per 1°C increase in temperature (Page et al., 2012).
5. Conclusions
We are facing an unprecedented rise in not one but three unique risk factors for heat-related illness and death: 1) Increasing global temperatures, 2) Increasing frequency, duration and intensity of extreme heat events and, 3) Increasing usage of a medication with potentially fatal heat-intolerant side effects. These facts have been independently confirmed through the UN Intergovernmental Panel on Climate Change, the National Center for Health Statistics and globally diverse research.
6. Recommendations
Several scientists have stepped forward to voice their concern over the interaction between antidepressant drugs and future climate change, with Martin-Latry et al. (2007) noting, “In special risk situations such as heat waves, the risk/benefit ratio of psychotropic drugs which could interfere with body temperature regulation has to be carefully assessed” (p. 335). Bark (1998) concurs, warning that during hot weather, “Medication, particularly anticholinergics, should be kept to the minimum, and benzodiazepines, rather than antipsychotic medications, should be used for agitation.” Stollberger et al. (2009) speak to the same issue, highlighting “an immediate need for public awareness during heat waves and for long-term strategies to mitigate the expected increase in future heat wave-related fatalities” (p. 879).
I believe that a significant number of heat-related deaths due to antidepressant use could be prevented if the public was better informed about the risks associated with psychotropic drug use. This goal could be accomplished through a combination of means, including: prominent labeling on all medication bottles, public service announcements (funded by drug manufacturers) during summer months and mandated warnings from medical professionals prescribing these drugs. However, limiting advisements to doctor/patient consultations would be ineffectual, as Pratt et al. (2011) note that only one half of patients taking antidepressants have visited their doctor in the last year. Pharmacy consultations, on the other hand, might offer a convenient opportunity to remind patients of their drug’s side effects when they arrive to refill their prescription. Affected patients could then exercise extra precautions during hot weather and, in the event of a heat wave and under the close supervision of a doctor, possibly decrease their dosage or discontinue antidepressant use temporarily.
Discussing research showing that prescription of antipsychotic medication was associated with an increased risk of death during extreme heat events, Page et al. (2012) warn,
“Given that global temperatures will continue to rise and the frequency of heat waves is predicted to increase in the years to come, these findings suggest that consequences of climate change may be felt disproportionately by people with mental illness” (p. 489).
In order to protect this already vulnerable population, I believe the medical community has an urgent responsibility to educate the public regarding the heat-intolerant side effects of antidepressant medication. As the IPCC (2007) reminds us, the warming of our climate is unequivocal, and the use of medication that could be adversely affected by such warming is unprecedented (National Center for Health Statistics, 2010). Warning the public about the potentially fatal interaction of these two concepts is of immediate and necessary concern.
Editor’s note: Originally written in fulfillment of requirements for ENVR e-130: Global Climate Change, Timothy C. Weiskel, DPhil and William R. Moomaw, PhD, Harvard University, May 2013.
References
Bark, N. (1998). Deaths of psychiatric patients during heat waves. Psychiatric Services, 49(8). Retrieved from http://ps.psychiatryonline.org/article.aspx?articleID=81739
Berry, H.L., Bowen, K., & Kjellstrom, T. (2010). Climate change and mental health: A causal pathways framework. International Journal of Public Heath, 55, 123-132. doi:10.1007/s00038-009-0112-0
Butcher, J., Hooley, J., and Mineka, S. (2010). Abnormal Psychology (14th ed.). Boston: Allyn and Bacon.
Centers for Disease Control and Prevention. (1998). Heat-related mortality – United States, 1997. Morbidity and Mortality Weekly Report, 47(23), pp. 473-476. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/00053616.htm
Doherty, T.J., & Clayton, S. (2011). The psychological impacts of global climate change. American Psychologist, 66(4), 265-276.
Epstein, Y., Albukrek, D., Kalmovitc, B., Moran, D.S., & Shapiro. (1997). Heat intolerance induced by antidepressants. Annals of the New York Academy of Sciences, 813, 553-558. doi:10.1111/j.1749-6632.1997.tb51746.x
Gaffen, D.J. & Ross, R. (1998). Increased summertime heat stress in the U.S. Nature, 396, pp. 529 –30.
Gitlin, M.J. (2002). Pharmacological treatment of depression. In I.H. Gotlib & C.L. Hammers (Eds.), Handbook of depression, 360-382. New York: Guilford.
Hansen, A., Bi, P., Nitschke, M., Ryan, P., Pisaniello, D., & Tucker, G. (2008). The effect of heat waves on mental health in a temperate Australian city. Environmental Health Perspectives, 116(10), 1369-1375. doi:10.1289/ehp.11339
Intergovernmental Panel on Climate Change. (2007). Summary for Policymakers. Climate Change 2007: Synthesis Report. Retrieved from http://www.ipcc.ch/pdf/assessment-report/ar4/syr/ar4_syr_spm.pdf
Kudoh, A., Takase, H., & Takazawa, T. (2003). Chronic treatments with antidepressants decreases intraoperative core hypothermia. Anesthesia & Analgesia, 97, 275-279. doi:10.1213/01.ANE.0000068821.29712.AC
Luber, G., & McGeehin, M. (2008). Climate change and extreme heat events. American Journal of Preventative Medicine, 35(5), 429-435. doi:10.1016/j.amepre.2008.08.021
Martin-Latry, K., Goumy, M-P., Latry, P., Gabinski, C., Begaud, B., Faure, I., & Verdoux, H. (2007). Psychotropic drugs use and risk of heat-related hospitalization. European Psychiatry, 22, 335-338. doi:10.1016/j.eurpsy.2007.03.007
Meltzer, H.Y. & Maes, M. (1995). Effects of ipsapirone on plasma cortisol and body temperature in major depression. Biological Psychiatry, 38, pp. 450 – 457.
Page, L.A., Hajat, S., Kovats, S., & Howard, L.M. (2012). Temperature-related deaths in people with psychosis, dementia and substance misuse. The British Journal of Psychiatry, 200, 485-490. doi:10.1192/bjp.bp.111.100404
Pratt, L.A., Brody, D.J. & Qiuping G. (2011). Antidepressant Use in Persons Aged 12 and Over: United States, 2005-2008. Centers for Disease Control and Prevention. Retrieved from http://www.cdc.gov/nchs/data/databriefs/db76.pdf
Ruosteenoja, K., Carter, T.R., Jylha, K. & Tuomenvirta, H. (2003). Future climate in world regions: an intercomparison of model-based projections for the new IPCC emissions scenarios. Helsinki: Finnish Environment Institute, 83.
Stollberger, C., Lutz, W., & Finsterer, J. (2009). Heat-related side-effects of neurological and non-neurological medication may increase heatwave fatalities. European Journal of Neurology, 16, 879-882. doi:10.1111/j.1468-1331.2009.02581.x
Wozniak, K.M., Aulakh, C.S., Hill, J.L. & Murphy, D.L. (1988). The effect of 8-OH-DPAT on temperature in the rat and its modification by chronic antidepressant treatment. Pharmacology Biochemistry and Behavior, 30, pp. 451-456.
My post publishing schedule is super random (I really need to work on that! lol)
So if you don’t wanna miss new articles, feel free to enter your email address below and we’ll shoot you a message when new posts go live :) ♥
*Please note: You’ll receive an email asking you to confirm your subscription. Make sure you open and click confirm – otherwise, you won’t get updates! :)
You can also find Prayers and Apples on the social media sites below! ♥
Other Posts You Might Like:
- Positive Psychology: The Science of Beyonce
- How to Be Optimistic (Like a Boss)
- Gluten and Depression: The Jimi Hendrix Experience
- What Percent of Happiness Can We Control?
- Exercise and Mood: The Basics
- ADHD, Autism and the Gluten Connection
- Depression Research Everybody Deserves to Know
- Can You Really Die from a Broken Heart?







Holy cow! Some of this information I had no idea about… I can remember going to the dr due to my hands shaking and her prescribed something for anxiety…(I know you’re shocked….lol!) but sure enough it was and after taking something for a time they stopped.
“Recognizing the relationships between serotonin/dopamine and thermoregulation/thirst regulation and serotonin/dopamine and mood disorders, provides a general framework for understanding some of the ways in which antidepressant drugs (that manipulate serotonin/dopamine) could contribute to heat-related illness and/or death.”
This is really good info Jessica!!
Thanks for taking the time to read through! Only a couple more projects to go and this semester is over :) This one was for a class on climate change… I had to find some way to put a Prayers and Apples twist on it, so this is what I came up with lol And you, anxious?? Nooooo ;) lol
Hey Jessica, not sure if you remember me. I am the friend of your mom’s from Relay For Life. I have met you and your brother there as well. She gave me one of your cards for your blog and now I am hooked. I am amazed at the research that you put into all of your blogs. I’ve been trying to catch up on some of your earlier posts. Good luck on all your end of semester obligations. I like the way you tie them into your blog.
Hi Judy! I do remember you – and my mom showed me a fun picture of you two at this year’s Relay! :) Thanks so much for stopping by, I’m glad you enjoy the posts! And thanks for the well wishes – I’ll be happy once I get all of my papers out of the way :) Thanks again for reading!
Fantastic, informative, well written, easy to read. I just love the way you write and this has great information I needed to know. Thank you times three!
You’re so welcome! Thanks for stopping by! :)