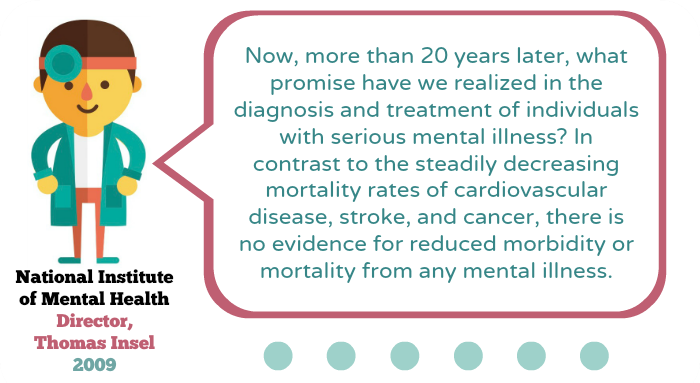
Since the introduction of Prozac, disability rates due to mental illness have more than doubled. Antidepressant use has increased 400%, yet morbidity and mortality rates due to mental illness haven’t decreased. At all.
For the past three years, I’ve tried to figure out why…
And I’m not alone. Some pretty big names have highlighted the same question – with many dedicating entire books to the subject. (See: Joseph Glenmullen, Clinical Instructor in Psychiatry at Harvard Medical School, Marcia Angell, former editor-in-chief of The New England Journal of Medicine, Irving Kirsch, Associate Director of the Placebo Studies Program at Harvard Medical School… you get the drift…)
I founded Prayers and Apples as a way to explore this question and promote evidence-based conversations about mental health. However – in the process – I discovered some pretty crazy stuff. For instance:
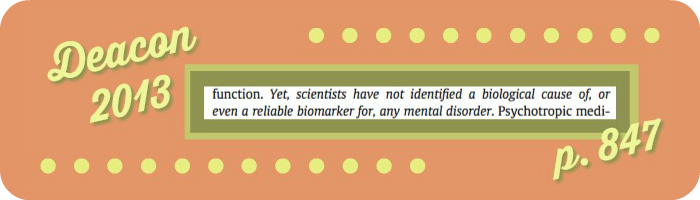
Researchers have never identified a biological cause of, or reliable biological marker for, any mental disorder…
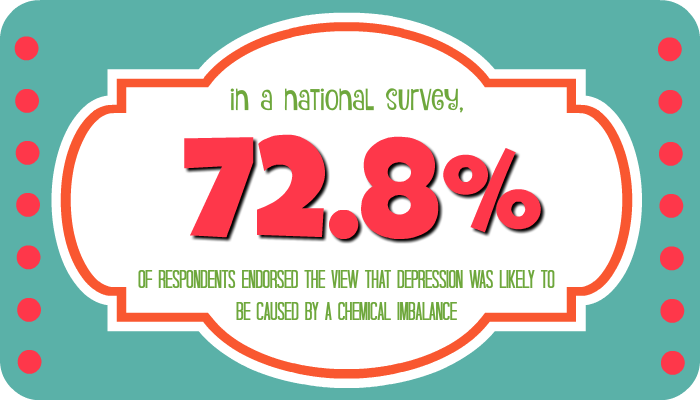
…yet the majority of Americans believe depression is a neurobiological disease.
Kinda strange, right?
The whole idea that depression is caused by a chemical imbalance is an unconfirmed hypothesis that has never been found to be true. (In fact, there’s a bunch of work disproving it.) Yet, a 2007 survey of undergraduate psychology students revealed that 84.7% viewed “chemical imbalance” as a potential cause of depression.
Now consider this: psychosocial interventions (such as exercise, spirituality, and therapy) have been shown to be super effective at treating depression – yet their use has steadily decreased as our nation’s mental health crisis has gotten worse.
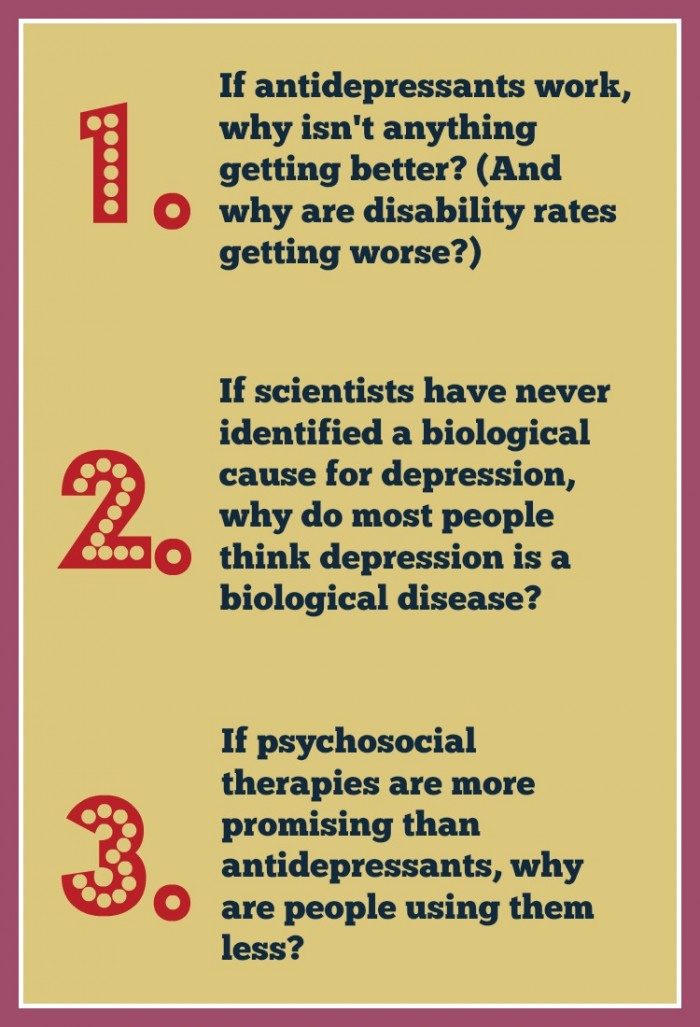
So we’re left with three mysteries:
(For my fellow research nerds, here’s the same info with citation links):
1. Antidepressants are the most popular treatment for depression. Yet, since their debut, mental illness morbidity and mortality rates haven’t improved. On top of that, disability rates due to mental illness have more than doubled. (Note: While temporal proximity does not prove that increased use of pharmaceutical medication is responsible for rising disability rates, Deacon has suggested that the possibility is “sufficiently plausible” to warrant serious investigation.)
2. Scientists have never identified a biological cause for depression. Yet, most Americans think depression is a biological disease. As summarized by Moncrieff and Cohen: widespread use of psychiatric drugs is justified by the idea that antidepressants work by helping to correct underlying biological abnormalities. However, there is no evidence that this is true.
3. Research has highlighted the effectiveness of psychosocial interventions (like exercise, spirituality, and therapy) but, as America’s mental health epidemic has gotten worse, use of psychosocial therapies has declined.
Why all of this is important
Belief in the chemical imbalance theory has been shown to (1) increase confidence in antidepressants (a treatment that – as just discussed: doesn’t have the best track record), and (2) decrease confidence in psychosocial interventions (which, as described by Thomas Insel, Director of the National Institute of Mental Health: are “arguably more encouraging”).
On a broader level (note: this is my own argument): Deferment to the biological model of depression compromises the ability of patients to exercise ethically informed treatment consent.
Research everyone deserves to know
To address this concern, I began thinking about marketing strategies that could effectively communicate evidence-based data to patients, to help support more informed treatment decisions (such as the #HowDoYouKnow campaign).
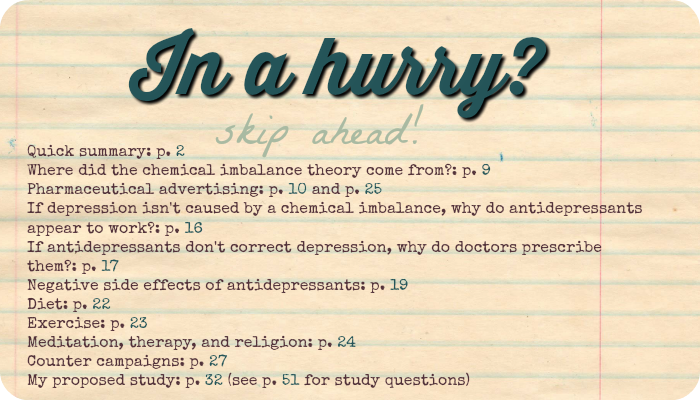
As part of a formal thesis, I developed my ideas under the guidance of neuropsychologist, Dr. Stephanie Peabody (#hero). After tons of research (reviewing 200+ studies!) I’m so happy and excited to finally share everything I found:
Please feel free to scroll through (you’d don’t even have to leave this window!) or download, save, and share with friends! :)
In a nutshell…
For those of you who aren’t in a huge rush… but also don’t feel like reading the whole PDF (no worries!)… I’ve copied and pasted my closing paragraphs below. (Sometimes you can get a great feel for a book by reading its last page, so hopefully this does the trick!)

The present paper has argued that lay perception of depression etiology is shaped by the biomedical model (France et al., 2007; Pescosolido et al., 2010) – most commonly expressed via the chemical imbalance theory – and that deferment to this paradigm promotes favoritism of pharmaceutical treatment (Deacon & Baird, 2009) and discourages use of psychosocial interventions (Kemp et al., 2014). I’ve suggested that this set of attitudes, in turn, results in patient harm by (a) subjecting patients to negative side effects (i.e., Antonuccio et al., 1999; Healy, 2003) that might otherwise be avoided through use of non-pharmaceutical treatments, and (b) preventing patients from experiencing potentially more positive treatment outcomes afforded by alternative, psychosocial interventions (Blumenthal et al., 1999; Bonelli et al., 2012). I’ve suggested that faith in the chemical imbalance theory promotes further harm by encouraging patients to base beliefs regarding depression etiology, prognosis, and treatment expectancy on unsubstantiated claims.
Arguments for a pharmaceutical counter-campaign (Gallo et al., 2013; Gaudiano & Miller, 2013) – including DTCA (Santucci et al., 2012) and counter-detailing (Avorn & Soumerai, 1982) – have been supported as a viable solution to this problem. I have proposed a novel starting point for practical application (i.e., campaign strategy/content development): deconstruction of the chemical imbalance theory – and have argued that overcoming better financed pharmaceutical campaigns (Donohue et al., 2007) is possible if this strategy is executed by organized efforts within the medical community. To support this claim, I have proposed a nationally representative survey to extend the work of Kemp et al. (2014) and France et al. (2007). The proposed study seeks to gauge lay belief in the chemical imbalance theory and correlate this perception with attitudes regarding five specific psychosocial interventions (including: diet, exercise, meditation, psychotherapy, and spiritual/religious practices). It is hypothesized that results will support the present argument – finding that belief in the chemical imbalance theory is key to shaping lay perception of depression treatment. This evidence will, hopefully, provide researchers with a strengthened foundation for developing future counter- campaigns.
As a point of clarity, the value of antidepressant use, in certain cases, has not been disputed. However, this value is argued to be best understood through frameworks presented by Breggin (2015) and Moncrieff and Cohen (2009) – that is, perceived therapeutic benefits are the result of a drug-induced, altered state of mind; antidepressants do not “work” by addressing neurochemical substrates of depression. This distinction highlights an ethical claim propelling the present thesis: Patients have a right to base treatment decisions on truly informed consent.
Consumers are empowered to take control of their lives when they are “knowledgeable about what works to solve a problem” (Sanders & Kirby, 2012, p. 240). Patients are likely to respond differently to an offer of a drug intended to produce an altered state of mind than a drug said to act on the underlying biological cause of depression (Moncrieff & Cohen, 2009). However, most patients are never given this choice. A significant part of recovery involves telling stories about depression and the self that “allow one to go on living” (Ridge & Ziebland, 2006, p. 1050) – yet, a majority of today’s stories are based on false truths (Cohen & Hughes, 2011).
If, after developing a more rational understanding of psychopharmaceutical drugs, patients still choose to take antidepressants, then it is the position of this paper that they should be free to do so. However, if just one patient – out of the estimated 60 million Americans who take psychotropic medication (Medco Health Solutions, 2011 as cited by Deacon, 2013) – would change their mind based on the evidence presented today, then it is firmly argued that organized psychiatry has an ethical obligation to communicate this information. As warned by France et al. (2007): “Any unitary understanding of human suffering asserted in isolation of its nuances, may mislead those in need of treatment and confound self-understanding” (p. 411). We do not know how psychology/biology causation works – and there are serious costs to pretending that we do (Miller, 2010).
Critiquing the chemical imbalance theory – and the biomedical model that it represents – is no more an affront to disorder management than criticizing a campaign that claims headaches are caused by a lack of aspirin in the brain. To the contrary, advocating for an evidence-based understanding of depression supports ethically informed treatment decisions and appropriate use of therapies that might otherwise be avoided. It relaxes blinders placed on research, that may neglect promising but anti-theory evidence, and encourages a rightfully curious approach to scientific inquiry.
Cohen and Hughes (2011) have noted that, “it remains completely unclear who will expose laypersons and professionals to messages that encourage critical thinking about psychoactive drug effects and the origin and relief of psychological distress” (p. 183). To this point, I direct attention to Healy (1987): Change is likely to come from those new to a field, who by virtue of youth, or transfer from another discipline or by some other method have escaped the usual moulding (sic) pressure and who are more struck by what is not explained by the dominant view than by its improvements on previous views (p. 350).
The present paper has attempted to highlight the brave work of researchers who have challenged the biomedical model of depression. It is my hope that the proposed study will contribute, in some small way, to this literature. There is currently no known biological cause of, or biological marker for, any mental disorder (Deacon, 2013) – yet, the majority of Americans believe depression is a confirmed, neurobiological disease (Link et al., 1999). It is the ethical responsibility of the medical community to correct this misconception. As argued by Miller (2010): “Intellectual modesty is in order” (p. 717).
Thank you so much for reading!
My goal in organizing this research is to promote positive, evidence-based patient education. So please don’t hesitate to contact me if you have any questions at all! :)
And if you found today’s post interesting, please feel free to share! ♥ Patients deserve an open, honest, scientifically based discussion about all types of depression treatment – so let’s get a conversation going! :)
Thanks so much for reading!!
xo Jessica
References *for post citations only – see PDF for full research references
Antonuccio, D.O., Danton, W. G., DeNelsky, G. Y., Greenberg, R. P., & Gordon, J. S. (1999). Raising questions about antidepressants. Psychotherapy and Psychosomatics, 68, 3-14.
Avorn, J. & Soumerai, S.B. (1982). Use of computer-based Medicaid drug data to analyze and correct inappropriate medication use. Journal of Medical Systems, 6(4), 377-386.
Blumenthal, J.A., Babyak, M.A., Moore, K.A, Craighead, W.E., Herman, S., Khatri, P.,…Krishnan, P.R. (1999). Effects of exercise training on older patients with major depression. Archives of Internal Medicine, 159(19), 2349-2356.
Bonelli, R., Dew, R.E., Koenig, H.G., Rosmarin, D.H., & Vasegh, S. (2012). Religious and spiritual factors in depression: review and integration of the research. Depression Research and Treatment, 2012, Article ID 962860.
Breggin, P.R. (2015). Rational principles of psychopharmacology for therapists, healthcare providers and clients. Journal of Contemporary Psychotherapy, 1-13.
Cohen, D. & Hughes, S. (2011). How do people taking psychiatric drugs explain their “chemical imbalance?”. Ethical Human Psychology and Psychiatry, 13, 176e189.
Craft, L.L. & Perna F.M. (2004). The benefits of exercise for the clinically depressed. Primary Care Companion to the Journal of Clinical Psychiatry, 6(3), 104-111.
Deacon, B.J. (2013). The biomedical model of mental disorder: a critical analysis of its assumptions, consequences, and effects on psychotherapy research. Clinical Psychology Review, 33, 846e861.
Deacon, B. J. & Baird, G. L. (2009). The chemical imbalance explanation of depression: Reducing blame at what cost? Journal of Clinical and Social Psychology, 28(4), 415– 435.
Delgado, P.L. (2000). Depression: The case for a monoamine deficiency. Journal of Clinical Psychiatry, 61(Suppl. 6), 7-11.
Dobson, K.S. (1989). A meta-analysis of the efficacy of cognitive therapy for depression. Journal of Consulting and Clinical Psychology, 57(3), 414-419.
Donohue, J.M., Cevasco, M., & Rosenthal, M.B. (2007). A decade of direct-to-consumer advertising of prescription drugs. New England Journal of Medicine, 357, 673-681.
Dubvosky, S., Davies, R., & Dubvosky, A. (2003). Mood disorders. In R. Hales & S. Yudofsky (Eds.), The American Psychiatric Textbook of Clinical Psychiatry (4th ed.), (pp. 439- 542). Washington, D.C.: American Psychiatric Press.
France, C.M., Lysaker, P.H. & Robinson, R.P. (2007). The “chemical imbalance” explanation for depression: Origins, lay endorsement, and clinical implications. Professional Psychology: Research and Practice, 38(4), 411-420.
Gallo, K.P., Comer, J.S., & Barlow, D.H. (2013). Direct-to-consumer marketing of psychological treatments for anxiety disorders. Journal of Anxiety Disorders, 27(8), 793- 801.
Gaudiano, B.A. & Miller, I.W. (2013). The evidence-based practice of psychotherapy: Facing the challenges that lie ahead. Clinical Psychology Review, 33(7), 813-824.
Glenmullen, J. (2000). Prozac backlash: Overcoming the dangers of Prozac, Zoloft, Paxil and other antidepressants with safe, effective alternatives. New York, NY: Simon and Schuster.
Healy, D. (1987). The structure of psychopharmacological revolutions. Psychiatric Developments, 4, 349-376.
Healy, D. (2003). Lines of evidence on the risks of suicide with selective serotonin reuptake inhibitors. Psychotherapy and Psychosomatics, 72, 71-79.
Healy, D. (2015). Serotonin and depression: The marketing of a myth. British Medical Journal, 350, h1771.
Insel, T. (2009). Translating scientific opportunity into public health impact: A strategic plan for research on mental illness. Archives of General Psychiatry, 66(2), 128-133.
Kemp, J.J., Lickel, J.J., & Deacon, B.J. (2014). Effects of a chemical imbalance casual explanation on individuals’ perceptions of their depressive symptoms. Behaviour Research and Therapy, 56, 47-52.
Link, B. G., Phelan, J. C., Bresnahan, M., Stueve, A., & Pescosolido, B. A. (1999). Public conceptions of mental illness: Labels, causes, dangerousness, and social distance. American Journal of Public Health, 89, 1328-1333.
Medco Health Solutions. (2011). America’s state of mind. Retrieved January 4, 2016.
Miller, G.A. (2010). Mistreating psychology in the decades of the brain. Perspectives on Psychological Science, 5(6), 716-743.
Moncrieff, J. & Cohen, D. (2009). How do psychiatric drugs work? British Medical Journal, 338, b1963.
Olfson, M., Marcus, S.C., Druss, B., Elinson, L., Tanielian, T., & Pincus, H.A. (2002). National trends in the outpatient treatment of depression. Journal of the American Medical Association, 287, 203-209.
Pescosolido, B.A., Martin, J.K., Long, J.S., Medina, T.R., Phelan, J.C., & Link, B.G. (2010). A disease like any other? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. The American Journal of Psychiatry, 167, 1321- 1330.
Pratt, L.A., Brody, D.J., & Qiuping, Gu. (2011). Antidepressant use in persons aged 12 and over: United States, 2005-2008. Centers for Disease Control and Prevention: NCHS Data Brief, No. 76.
Ridge, D. & Ziebland, S. 2006. “The old me could never have done that”: How people give meaning to recovery following depression. Qualitative Health Research, 16(8), 1038- 1053.
Sanders M.R. & Kirby, J.M. (2012). Consumer engagement and the development, evaluation, and dissemination of evidence-based parenting programs. Behavior Therapy, 43, 236- 250.
Santucci, L.C., McHugh, R.K., & Barlow, D.H. (2012). Direct-to-consumer marketing of evidence-based psychological interventions: Introduction. Behavior Therapy, 43, 231- 235.
Whitaker, R. (2010). Anatomy of an epidemic: Magic bullets, psychiatric drugs, and the astonishing rise of mental illness in America. New York, NY: Broadway Books.







Such informed research, great work! You certainly have a hit in this one – keep going…..
Thank you!! :)
Hi,
Thank you for the info! So, if antidepressants aren’t the answer, what is? A clean diet? What do I do?
Hi Gretchen,
So glad you enjoyed the post! Scientists and doctors are still working diligently to answer that very question, but at the present time there are a number of psychosocial options (such as talk therapy/counseling, exercise, meditation) that offer a lot of hope! I’d encourage you to read pages 22-24 of the embedded research report for a more detailed overview of each area. The Resource links (in the right-hand column) also offer a lot of great information from research-based institutions :) As I’m not a doctor myself, I’ve organized a separate post on finding doctors that embrace an integrative approach to health and healing (click here). Hopefully this will be of help! Please let me know if you have any additional questions! :)
good work! the pharmaceutical industry has promulgated the “chemical imbalance” theory so that they can answer a question that no one would be asking by saying that their proprietary, patented, highly profitable drugs are the answer to “how do we treat the chemical imbalance that causes depression”? they spend big money selling this fiction because they make HUGE money with their “solution”. their propaganda has now attained the status of gospel, and may God sincerely protect those who suffer, from these self-professed “saviors” who will endanger their lives and do damage to the sufferers’ quality of life in the pursuit of the almighty buck. here’s a recent piece speaking to something similar: “Does Medication Actually Make Us Live Longer?” https://www.huffingtonpost.com/entry/medication-live-longer-longevity_us_5c1a9231e4b0ce5184b9bcc1
Glad you enjoyed and thanks so much for taking the time to comment! :)